Intro into Mobile Radiography
In a world where instant access defines success, mobile radiography is revolutionising how we deliver diagnostic imaging—bringing the X-ray machine directly to the patient’s bedside. Whether it’s an ICU patient too critical to move or a busy emergency department requiring quick answers, mobile imaging is the unsung hero of modern medical diagnostics.
But what exactly is mobile radiography, and what do you need to know to master it?
🚑 What is Mobile Radiography?
Mobile radiography refers to diagnostic X-ray imaging performed with portable X-ray equipment outside the traditional radiology department. This includes performing radiographic exams in:
- Hospital wards and intensive care units (ICU)
- Emergency departments
- Operating theatres
- Aged care facilities
- Rural and remote settings
Mobile imaging is essential for patients who are too unwell or immobile to be transported safely to the radiology department.
📘 Key Concepts and Terminology You Must Know
1. Mobile X-ray Unit
The machine itself is a powered x-ray device, designed for flexibility and portability. They’re equipped with a control panel, an X-ray tube, and a detector (either computed radiography (CR) cassettes or digital radiography (DR) flat panel detectors).

⚡ Catchy Insight: Not all heroes wear lead aprons—but they should. Mobile radiographers are frontline diagnostic responders.
2. Source-to-Image Distance (SID)
In mobile X-rays, SID consistency is crucial. Unlike fixed units with preset distances, mobile units rely on the radiographer’s skill to estimate and position accurately—commonly using 100 cm or 180 cm based on clinical need.

3. How to stay safe when the walls can’t protect you
Radiographers must be vigilant about radiation safety. Here are some of the methods they use to protect themselves from radiation:
- Scattered radiation control
- Shielding and distance
- ALARA principles (As Low As Reasonably Achievable)
- Signage and staff safety awareness
4. Patient Positioning Challenges
Working around:
- Medical equipment (e.g., ventilators, IV poles, ECG leads)
- Unconscious, uncooperative, or non-ambulant patients
- Inadequate lighting or space
Adept radiographers need to think three-dimensionally—and sometimes acrobatically—to get the best image with minimal patient disturbance.
5. Exposure Factors and Technique Modification
Some Variables that Radiographers modify in practice:
- Lack of a grid vs grid use
- Body habitus of patient and pathology that patient presents
- Angle of incidence (tube angulation)
- Receptor placement under challenging circumstances
Here’s an example of a control panel, showing the values for a standard chest xray. A good range for a chest would be from 80-140 kVp to penetrate the body and a low mAs, from 1-12 mAs.
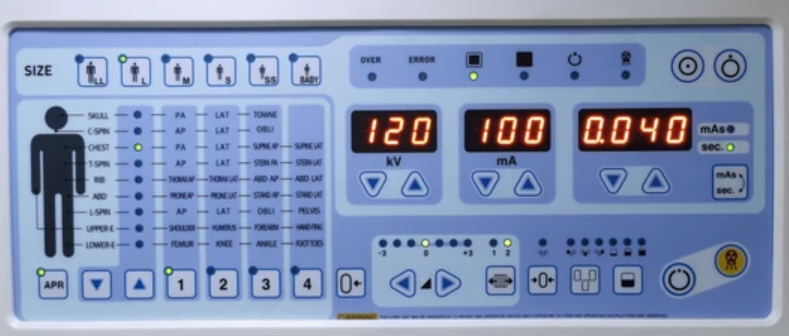
🎯 In mobile imaging, technique isn’t just about kVp and mAs —it’s about clever compromise of all the variables.
🧠 Why Is It More Than Just Pushing a Machine?
Mobile radiography demands:
- Critical thinking
- Patient-centered care
- Adaptability in high-pressure environments
- Interdisciplinary communication with nurses, doctors, and anaesthetists

💬 A mobile radiographer must be part radiographer, part diplomat, part detective!
🎓 Reflective Insight
Mobile radiography isn’t just about moving the machine—it’s about moving with purpose, precision, and empathy. As radiographers, we bring the power of diagnosis to the doorstep of the critically ill, playing a silent but vital role in patient outcomes.
So the next time you’re wheeling a unit down a dim hallway, remember: you’re not just taking a portable X-ray—you’re delivering life-saving insight, one image at a time.
KEEP ON READING Radiography Insights for MORE general information, clinical tips and behind-the-scenes perspectives from frontline imaging heroes.